Chest Pain: Is It Digestive Tracts?
Pathology in the upper digestive tract which are the esophagus and stomach can give rise to chest pain, though they are most commonly felt at the lower chest or upper abdomen area (epigastrium).
Common associated symptoms in esophagus disorders include dysphagia (difficulty in swallowing) & odynophagia (pain when swallwong), while in stomach disorders, abdominal bloating, nausea, vomiting, indigestion are common related symptoms.
Gastroesophageal Reflux Disease (GERD)
This condition is caused by back-flow of acidic stomach content back into the lower part of esophagus. There is a muscular "valve" between the lower esophagus and stomach which allows only one-way flow of food content from the esophagus towards the stomach. However, due to some condition, the "valve" does not function properly and allows the food to flow backwards.
There are many condition which can give rise to GERD, such as:
- pregnancy
- obesity
- prolonged/excessive straining over abdomen (coughing/vomiting/physical exertion)
- certain foods
- smoking
- hiatal hernia
The chest pain caused by GERD is typically referred to "heartburn", where the pain is "burning" in nature and radiate upwards towards the neck/throat. It may be accompanied by bitter taste in the mouth.
Esophagitis
Infection or inflammation of the esophagus can cause pain along the chest area. The pain may be made worse after food when the food bolus pass through the inflammed area.
Esophagus spasm
Either irregular or regular esophagus spasm can cause pain, mostly after food intake. It is not common and the cause is unknown. The pain is usually intermittent and can be severe.
Esophageal cancer
Esophageal cancer most commonly occurs at the lower part of esophagus and pain is not a usual symptom. Most sufferers will complain of dysphagia or food stuck at the lower part of the esophagus. More advanced case can give rise to poor appetite and weight loss, as in all type of cancers.
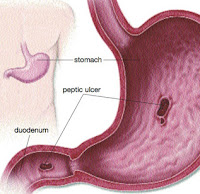
Peptic ulcer disease
This is a common disorder and is highly related to Helicobacter pylori infection, regular use of NSAIDs and blood-thinning drugs. The ulcers can be at the stomach or upper portion of the small intestines (duodenum). Besides pain over the chest (heartburn) or upper abdomen especially between meals and at night, sufferers may also complain of bloating, nausea & vomiting.
Peptic ulcers can be life-threatening if it is bleeding profusely. Thus, in case of chest discomfort accompanied by vomiting blood (hematemesis) or passing black stool (melena) or anemia (pale), the patient has to seek medical attention immediately.
Gastritis
Gastritis is a term used to described inflammation or irritation of stomach lining. It is a common diagnosis made by doctors for upper abdominal pain. The pain can be felt at chest area as heartburn with abdominal bloating, nausea & vomiting. The causes and symptoms of gastritis are similar to peptic ulcer disease. Doctors can only differentiate both of them by doing an oesophageal-gastro-duodenal-scopy (OGDS).
Click here for clues on how to differentiate chest pain.
Click here for clues on how to differentiate chest pain.